Lung cancer remains the leading cause of cancer-related deaths globally, with non-small cell lung cancer (NSCLC) accounting for the vast majority of cases. While chemotherapy is often the first line of defense, its effectiveness is increasingly limited by toxic side effects and growing drug resistance. The key problem is that chemotherapy also weakens the immune system, making it harder for the body to fight cancer long-term. Tumors actively suppress immunity by hijacking immune cell energy sources, leaving patients with fewer options.
Recent research offers a potential solution: directly boosting immune cell energy by transplanting functional mitochondria. This approach, published in Cancer Biology & Medicine by scientists at Tongji University and Nantong University, could restore the immune system’s ability to fight NSCLC while also making tumors more susceptible to chemotherapy.
How Mitochondrial Transfer Works
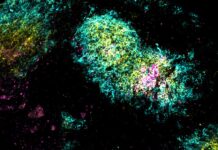
Researchers took functional mitochondria from healthy human heart cells (cardiomyocytes) – known for their high energy output – and transplanted them into NSCLC tumor models. The mitochondria alone had no effect on cancer cells, but when combined with the chemotherapy drug cisplatin, they dramatically amplified its effectiveness. The treatment reduced the amount of cisplatin needed to kill cancer cells by half, shrinking tumors more aggressively in mice and increasing immune cell infiltration.
This isn’t just about brute force; mitochondrial transfer fundamentally shifts the tumor’s metabolism. It reverses the “Warburg effect” – where cancer cells favor inefficient energy production – forcing them to rely on efficient oxidative phosphorylation. This weakens the tumor while simultaneously energizing immune cells, including T cells and natural killer cells.
Reversing Immune Suppression
The study also showed that mitochondrial transfer restored mitochondrial activity in immune cells, allowing them to function at full capacity. This is critical because chemotherapy often damages these cells, leaving patients vulnerable to relapse. Crucially, the treatment didn’t increase toxicity, preserving organ health and body weight.
“By replenishing immune cells with functional mitochondria, we are not just enhancing their energy – but restoring their ability to fight,” explains Dr. Liuliu Yuan, lead investigator. “At the same time, tumor cells become more vulnerable to chemotherapy. It’s like rearming the immune system while disarming the tumor.”
Implications for Future Cancer Treatment
This research suggests a new therapeutic paradigm: integrating mitochondrial transfer with existing cancer treatments to overcome immune suppression and metabolic resistance. While further clinical trials are needed, this approach holds promise not just for lung cancer, but potentially for other cancers where immune dysfunction is a major barrier to success. The ability to energize both the immune system and chemotherapy drugs could reshape cancer care, moving beyond current limitations and into a new era of bioenergetic restoration.